An academic version of this blog post, that explains why epitope redundancy provides resiliency (to bacteria) and weakness (to immune defense) can be found here.
. . . So a guy named Elledge has discovered a way to test your blood for the viruses that you’ve been exposed to. Sounds as if it will soon be available for doing at home, like a pregnancy test. What will you do if your test turns up positive for HIV? Will you freak out and call your ex-boyfriend? Or run for the nearest doc-in-a-box? That’s when it’s time to remember that redundancy is the immune system mantra, and that HIV has built its nest within it. And so has Hepatitis C, and Epstein Barr Virus (EBV) and Herpes Simplex Virus (HSV) for that matter. And… as we have now published, so too, has Avian Flu (H7N9). Meaning that H7N9, and . . . HIV look like … other stuff, and can even look like you, sometimes, so, don’t hang your hat on that test! Antibody epitopes and T cell epitopes, the things that our immune system recognizes when it’s searching for bad bugs, can be sculpted, by viruses and bacteria. The really good escape artists, like HIV and TB, make their T cell epitopes look . . . like us.
That’s what we call “epitope redundancy” and it’s everywhere, now that we have a tool called JanusMatrix, to look for it. There’s much that we can learn from this weakness in the immune system armature – about ourselves, and about our pathogen enemies. What we learn about ourselves will be good for the development of better treatments for autoimmune disease, and what we learn about our pathogen enemies will lead to the development of better, more effective, safer vaccines.
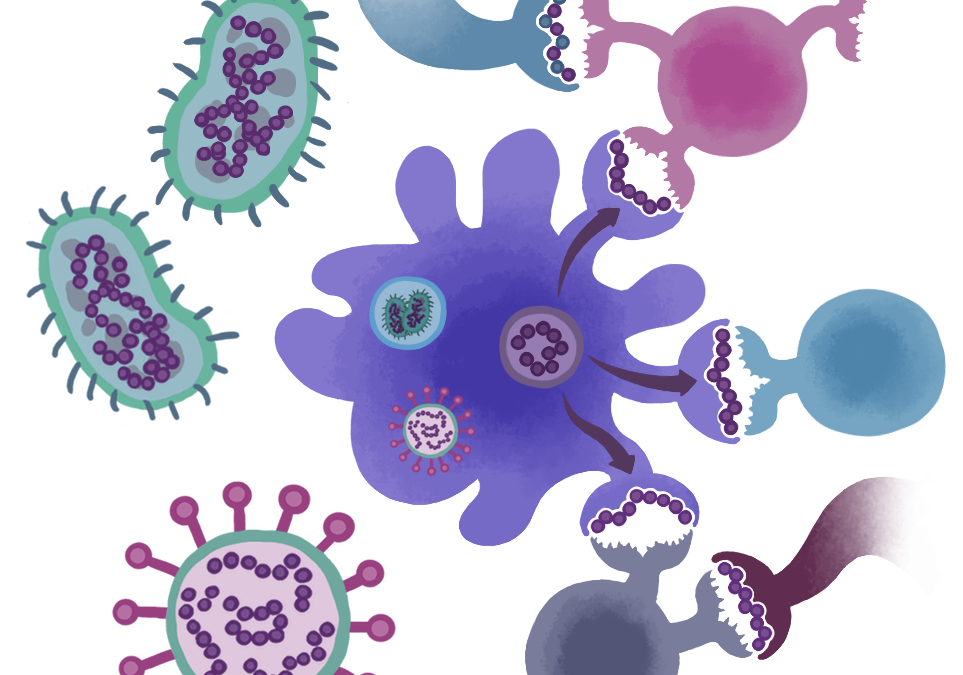
Pathogens have discovered myriad means of escaping immune response (some are reviewed in this nice article by Klenerman). This new concept – immune camouflage – was first described by our group in 2013, and now further evidence is emerging that HIV, HCV, EBV and HSV have built themselves a very successful niche, or nest, using bits and pieces of the human genome. By that we mean, the ‘immune signature’ of a virus is often indistinguishable from self. Viruses (and Bacteria and Parasites for that matter) have found ways to camouflage themselves, to reduce the likelihood that they will be identified, trapped, chewed up, spit out and eliminated by our humoral (antibody-based) and cellular (T cell) immune system. So how will are we able to tell Self from Pathogen, where in that thicket lies the truth?
As it turns out, it has been known for decades, if not centuries, that antibodies to pathogens cross-react with self proteins. We know that from syphilis, the ‘great masquerader’, because the original tests we had for ‘the clap’, also known as the VDRL and the RPR are based on detecting antibodies against Treponema pallidum but antibodies that react to Lyme, Malaria and yes, HIV, are cross-reactive with T. pallidum. I’ve always wondered what these important, and yet well camouflaged human diseases had in common: Why would a syphilis B cell epitope look like a Lyme disease epitope . . look like a self epitope? Well, of course, because the pathogen is doing its very best to camouflage itself from immune system attack. And it is no wonder, actually, that these same pathogens cause diseases that cause systemic symptoms, not unlike the total body malaise and aesthenia that we experience when we are given pooled human immune globulin, otherwise known as IVIG.
The same is true for T cells – we have found T cell epitopes that bind with the same affinity to certain HLA, derived from HIV and HCV, that look exactly like highly conserved T cell epitopes found in the human genome. Why are they there? Well, perhaps the fact that they are more common in pathogens that are commensal, such as EBV and HSV, provides a clue. In addition to deleting epitopes (known as immune escape, a strategy for which HIV is quite famous), these pathogens adopt T cell epitopes that look, on the T cell facing surface, just like common human T cell epitope. We have discovered that these epitopes may be suppressor, or regulatory T cell epitopes.
Cross-reactive T cell epitopes and immune regulation. These types of epitopes may be critically important for the regulation of immune response to self antigens, protecting key antigens from ‘auto’ destruction and attack. We have uncovered such epitopes in immunoglobulin, albumin, and other key immune system molecules (see our Tregitope publication page for more information). In these cases, pathogens such as commensal viruses, bacteria and parasites, may provide important clues to the regulation of auto-immunity.
Cross-reactive T cell epitopes and autoimmunity. But some of the epitopes that are cross-reactive between host and pathogen may not be regulatory T cell epitopes in the host. And so, are we surprised that these same commensal pathogens that use immune camouflage as a means of escape, are also associated with auto-immune disease syndromes? We think so, and so do a few other folks, who have uncovered uncanny resemblances between self and pathogens. The literature is replete with references. Here, and here, are a few, for example. Is there a lesson to be learned? Perhaps we should take those inflammatory cross-reactive epitopes out of vaccines.
That’s why we believe that it is high time that we learn from pathogens how to make better vaccines and biologics. Biomaterial scientists have been adopting lessons learned from pathogens to evade of immune responses to their products for decades. Can vaccinologists and immunologists . . . and rheumatologists and maybe also biologics developers also learn from immune camouflage? To be more precise, perhaps we should learn from viruses (and bacteria and parasites) which host epitopes they choose to imitate. Why do they camouflage themselves with one epitope (sometimes multiple pathogens use the same ‘self’ epitope) and not the other? Do those [human] epitopes play a key role in the regulation of human immune response? Putting those special epitopes into biologics, may reduce immune responses to the drugs, improving patient outcomes. And taking them out of vaccines, may result in better vaccines. What has proven to be a weakness in host defense, may be the hope that emerges, leading to solutions for unmet medical needs.